We survived a long day at the hospital yesterday. Longer hospital days are coming soon, however, so leaving yesterday afternoon for home was like an unspoken reprieve. Our top two priorites the next 8 days are, 1) enjoy our time at home thoroughly and intentionally, and 2) keep this boy healthy. The cardiac nurse practitioner in not so many words told us it would be crazy to send Luke to school next week. She also told Luke studies are finding that iPad use during procedures dramatically decreases the child's perception of pain and discomfort.
She is his new best friend.
And maybe insurance will cover a new iPad for Luke. We have studies, Regence!
Our day consisted of vitals, EKG, a chest X-ray, a lengthy meeting with the surgeon, a blood draw, a subsequent lengthy meeting with the cardiac nurse practitioner, a break for lunch, a visit to the pharmacy to pick up an antibiotic nose gel for the week before surgery, then finally, a consult with anesthesia.
Like we told the surgeon, this heart surgery rodeo is very, very different with a nine year old. Some good differences, some bad. I love that each person we came in contact with yesterday made Luke a part of the process, spoke directly to him, and let him ask any questions he had (not surprising to anyone who knows him that he had a few). That is most definitely a good difference. We have told him repeatedly leading up to this surgery that every nurse and doctor that walks into his room has two priorities: keep Luke as comfortable as possible, and get him home as quickly as possible. I think his interaction with the staff yesterday confirmed that for Luke. I think he trusts that these doctors and nurses have his best in mind. Even when they are asking him to do something really, really hard.
Another lesson relearned yesterday: We can laugh and be silly and those two things make everything seem a little better. Good attitudes really do go a long way.
Here is a bit more information from our surgical consult. And for all you visual learners, these are for you:
This is not an accurate graphic of Luke's heart, but it's a good visual of the DKS procedure that was done as part of his second open-heart surgery, and a good way to visualize where the stenosis is happening. The surgeon will incise the underside of the aorta, widen it, and place a cadaver homograft patch the length of the incision. There is a tiny chance Luke would have enough pericardial tissue to use for the patch, but unlikely. The only downside to the cadaver homograft is that it can increase Luke's antibodies, which would only be an issue if he needed a heart transplant down the road.
Here is what the repair basically looks like:
Dr. Chen told us it will be about a four hour procedure from start to finish. He will most likely come to the Cardiac ICU intubated but could be extubated within a couple of hours. The average ICU stay is two days and then he'll move to the surgical floor for the rest of his recovery.
I truly enjoyed meeting
Dr. Chen. It's rare to meet a heart surgeon who is not only good, but also personable and willing to connect. We spent at least 45 minutes talking after Roger and Luke left the room (also not surprising to anyone who knows me that I had a few questions myself. See note above about Luke's prolific question-asking ability). We are in good hands.
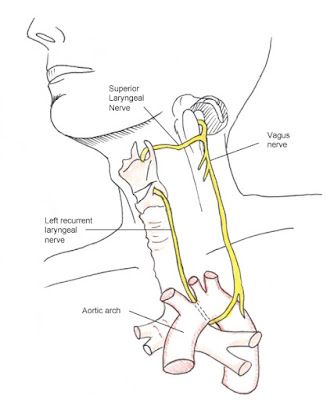
One thing I didn't know (and that we can be specifically praying against) is the high incidence of vocal cord nerve damage (about 15%) that can occur during aorta reconstruction. The laryngeal nerve runs right behind and underneath the aortic arch:
So, we are set for November 28. We have officially begun Mission: Stay
Healthy. I may or may not have crossed the line from oil lady to crazy
oil lady.
I'm okay with that.
We feel surrounded by so much love and support and we could not be more thankful to walk through this with all of you.